The term coronavirus refers to a large family of viruses that can cause illness in both animals and humans. In humans, coronaviruses commonly cause mild respiratory infections, such as the common cold. However, the world became intimately familiar with this family in late 2019 with the emergence of a highly infectious and novel strain: Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus responsible for Coronavirus Disease 2019 (COVID-19).
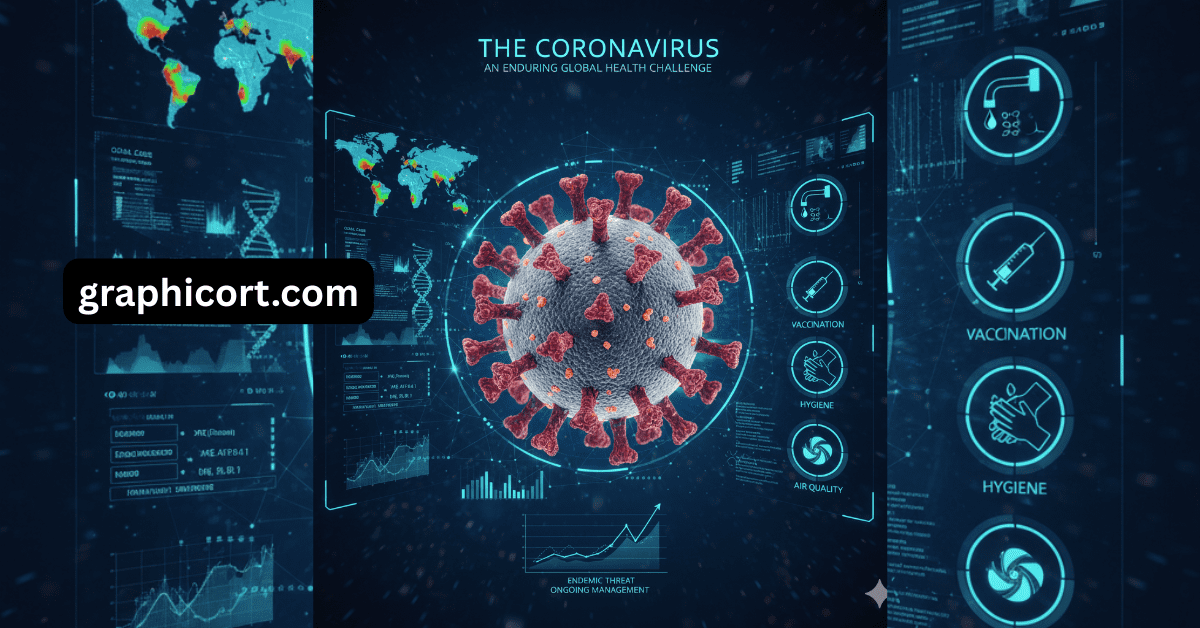
Although the global pandemic emergency phase has passed, the coronavirus remains an enduring public health threat that continues to evolve, necessitating ongoing vigilance, vaccination, and scientific research.
Understanding COVID-19 and Its Transmission
COVID-19 is a respiratory illness that ranges in severity from asymptomatic infection to mild cold-like symptoms, all the way to severe, life-threatening pneumonia and multi-organ damage.
Symptoms
Common symptoms of COVID-19 often resemble the flu or a bad cold, but can include:
- Fever or Chills
- Cough and Shortness of Breath or difficulty breathing
- Extreme Fatigue or tiredness
- Headache and Muscle or Body Aches
- Sore Throat
- New Loss of Taste or Smell (a unique symptom of earlier variants, less common now)
- Congestion, Runny Nose, Nausea, Vomiting, or Diarrhea
Symptoms typically appear 2 to 14 days after exposure to the virus. Older adults and people with underlying medical conditions (like heart disease, diabetes, or chronic respiratory issues) remain at the highest risk for severe illness, hospitalization, and death.
How It Spreads
SARS-CoV-2 is transmitted primarily through respiratory droplets and virus particles released into the air when an infected person breathes, talks, sings, coughs, or sneezes.
- Airborne Transmission: Infectious, tiny particles (aerosols) can linger in the air and accumulate in indoor spaces, especially those that are poorly ventilated.
- Close Contact: The risk of transmission is highest when people are in close proximity.
- Surface Contact (Less Common): The virus can also be spread by touching contaminated surfaces and then touching one’s eyes, nose, or mouth.
The Evolution of the Virus: Variants
Like all viruses, SARS-CoV-2 constantly changes (mutates) as it replicates. These changes lead to new variants, which can alter the virus’s characteristics, such as how easily it spreads or how well it can evade immune protection from previous infection or vaccination.
As of late 2025, the global focus has shifted from the initial waves (Alpha, Delta) to sublineages of the highly transmissible Omicron variant, such as XFG (Stratus) and NB.1.8.1, which are now dominant in many regions.
Public health organizations, like the WHO and CDC, continually monitor new strains, classifying them based on risk:
- Variant Under Monitoring (VUM): A newly detected variant with genetic changes that may pose a future risk.
- Variant of Interest (VOI): A variant with genetic changes that are predicted or known to affect transmission or severity.
While the virus continues to evolve, the current consensus is that existing treatments and updated vaccines remain effective at preventing the most serious outcomes—hospitalization and death.
Prevention and Protection
The most effective strategy against the coronavirus is a multi-layered approach that combines medical advances with responsible public health practices.
- Stay Up to Date with Vaccination: Vaccination remains the strongest protection against severe illness, hospitalization, and death. Vaccines are regularly updated to target the currently circulating variants.
- Practice Good Hygiene:
- Wash hands frequently with soap and water for at least 20 seconds.
- Cover coughs and sneezes with a bent elbow or tissue.
- Improve Air Quality: Increase ventilation in indoor spaces by opening windows or using air purifiers to reduce the concentration of viral particles.
- Isolate When Sick: If you have symptoms, stay home and away from others until you are fever-free for 24 hours (without fever-reducing medication) and your symptoms are improving overall.
- Seek Treatment: If you are at high risk for severe illness (age 65+, underlying conditions), contact a healthcare provider immediately after a positive test. Antiviral treatments can significantly lower the risk of severe illness if started within a few days of symptom onset.
The long-term impact of COVID-19 means the world must treat it as an endemic threat—a virus that circulates in the population, requiring continuous management, much like influenza. By staying informed and utilizing the tools developed by science, individuals can effectively mitigate their risk and protect vulnerable community members.